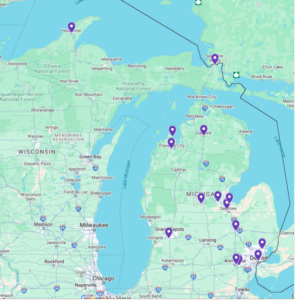
Image: Geographic Representation of 2025 CAPC MOQC Palliative Care Certificate Program Participants
Palliative care remains underutilized in Michigan, especially in oncology, due to persistent gaps in access. Patients across the state, particularly those in rural and tribal communities, often experience delays and poor outcomes caused by a shortage of trained providers, limited resources, and geographic isolation. To address these gaps, MOQC in partnership with the Center to Advance Palliative Care (CAPC), launched a six-month certificate program to equip clinicians with primary palliative care skills.
The program focuses on essential competencies such as pain and symptom management, communication, shared decision-making, and caregiver support. MOQC secured early buy-in from its Palliative Care and End-of-Life Task Force and announced the initiative at the January biannual meeting. The application process evaluated candidates on clinical background, geographic location, and dedication to palliative care. Applicants submitted a personal statement, description of educational goals, and a letter of support from their organization. Targeted outreach was conducted to engage providers in tribal communities. A transparent, rigorous scoring rubric ensured a fair and equitable selection process.
The response was strong. The program received 34 applications from a varied group of nurse practitioners (NPs), physician assistants (PAs), and medical doctors (MDs). Fifteen providers were selected for the inaugural cohort: eight NPs, six PAs, and one MD from a tribal health setting. Selections included providers from Michigan’s Upper Peninsula, a region with known gaps in palliative care access. The cohort’s variability, both geographically and professionally, ensures a broader statewide impact and supports the delivery of high-quality, person-centered care.
Initial lessons from the CAPC MOQC collaboration offer a model for replication: conduct targeted outreach to underserved communities, maintain a rigorous and transparent selection process, and foster partnerships with local organizations to broaden reach. Offering flexible, virtual learning options is crucial for accommodating busy clinical schedules. Ongoing participant feedback will guide improvements and measure the program’s long-term impact on care delivery.
In the initial months, the cohort has been fully engaged in the program. All participants completed their monthly training assignment and attended the first Virtual Clinical Discussion, which included a case-based conversation on applying new learnings in practice. To foster a sense of community learning, Basecamp was set up as a virtual classroom, where participants share examples of how they have begun to integrate aspects of palliative care into patient care. Their responses reflect a growing commitment to whole-person care, increased efforts to engage caregivers, and recognition of the importance of an interprofessional team. This group is fostering a collaborative and reflective learning environment that supports ongoing professional growth.